
News
The Zhejiang University Children's Hospital team’s latest research findings: Huperzine A shows promise in treating diabetic nephropathy.
Date:
26 Oct,2024
Recently, the renal medicine team from the Children's Hospital of Zhejiang University School of Medicine, in collaboration with Wanbangde Pharmaceutical Group Co., Ltd., published the latest findings of their multi-omics study on huperzine A for treating diabetic nephropathy. The research highlights huperzine A's promising therapeutic potential in alleviating diabetes-induced kidney damage, lipid metabolism disorders, and inflammation. The study was featured in the journal *Pharmacological Research*, under the full title "Huperzine A targets Apolipoprotein E: A potential therapeutic drug for diabetic nephropathy based on omics analysis."
As early as 2020, the Children's Hospital of Zhejiang University School of Medicine collaborated with Wanbangde Pharmaceutical Group Co., Ltd. to conduct a study evaluating the efficacy and safety of bromhexine hydrochloride tablets in treating children infected with the novel coronavirus. Now, the two organizations have joined forces once again, achieving promising results in a new disease area.
Huperzine A: Nature's Versatile Gift
Huperzine A (Hup A), an extract from the Asian plant *Huperzia serrata*, is clinically primarily used for treating neurodegenerative diseases. However, recent studies have revealed that it also exhibits significant antihyperglycemic and anti-inflammatory effects in diabetic retinopathy. Yet, its broader protective roles—particularly its potential to safeguard renal function in diabetic nephropathy, a common complication of diabetes—remain largely unexplored.
Diabetic Nephropathy: The Silent, Lurking Health Threat
Diabetes mellitus (DM), a common and widespread disease, is a global public health issue that poses a serious threat to human health. Today, the prevalence and number of people living with diabetes are rapidly increasing worldwide. According to statistics from the International Diabetes Federation (IDF), in 2021, the global adult population with diabetes reached 537 million—nearly a 16% rise compared to 2019. By 2045, the total number of people with diabetes worldwide is projected to climb to 783 million. In 2021, diabetes-related deaths worldwide totaled 6.7 million.
Over the past four decades, China has experienced rapid economic growth, a Westernization of lifestyles, urbanization, an aging population, and rising obesity rates—factors that have all contributed to a sharp increase in the prevalence of diabetes. In 1980, the adult diabetes prevalence in China was just 0.67%, but by 2007, it had climbed to 9.7%, and by 2017, it had surged even higher—to 11.7%. What’s more, the proportion of people with pre-diabetes is even greater. Alarmingly, nearly 50% of diabetes cases in China remain undiagnosed, while among those who are already receiving treatment, diabetes control remains far from optimal. According to IDF data, as of 2021, the number of adults with diabetes in China reached 141 million, firmly establishing the country as the nation with the largest diabetic population in the world.
Diabetic nephropathy (DN) is one of the most significant and severe complications of diabetes, with a complex pathogenesis involving oxidative stress, inflammation, fibrosis, and apoptosis. Clinically, it is characterized by persistent increases in albuminuria and a progressive decline in glomerular filtration rate (eGFR), ultimately leading to end-stage renal disease (ESRD). At this stage, kidney function is nearly completely lost, progressing to renal failure, where harmful toxins accumulate in the body, disrupting fluid, electrolyte, and acid-base balance—conditions that are highly dangerous and carry a significantly high mortality risk.
Currently, clinical treatment for diabetic nephropathy primarily focuses on early control of blood sugar and blood pressure. In advanced stages, however, therapies such as dialysis or other kidney replacement options become necessary. Unfortunately, there are currently no effective pharmacological interventions available.
Multi-omics analysis: Unveiling the mechanisms of huperzine A Mechanism of action
In this study, researchers employed a multidisciplinary, multi-omics approach—integrating transcriptomics, metabolomics, microbiome analysis, and network pharmacology—to investigate the therapeutic effects of huperzine A on diabetic nephropathy. The findings reveal that huperzine A exerts protective actions on the kidneys, modulates metabolism, reshapes the gut microbiota, and alleviates inflammation by regulating ApoE expression. This research provides, for the first time, compelling evidence supporting huperzine A's therapeutic potential in treating DN, suggesting that it could serve as a promising candidate for both preventing and treating diabetic nephropathy by specifically targeting and modulating ApoE. Specifically:
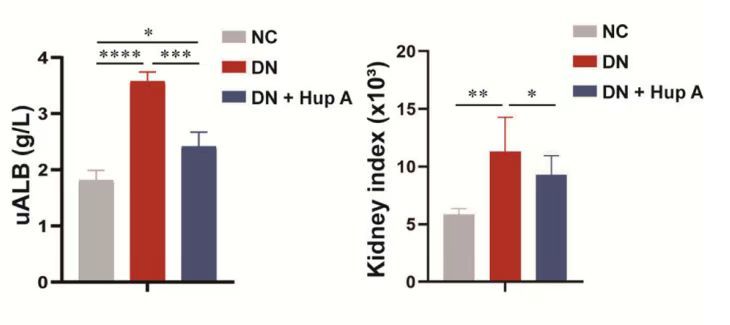
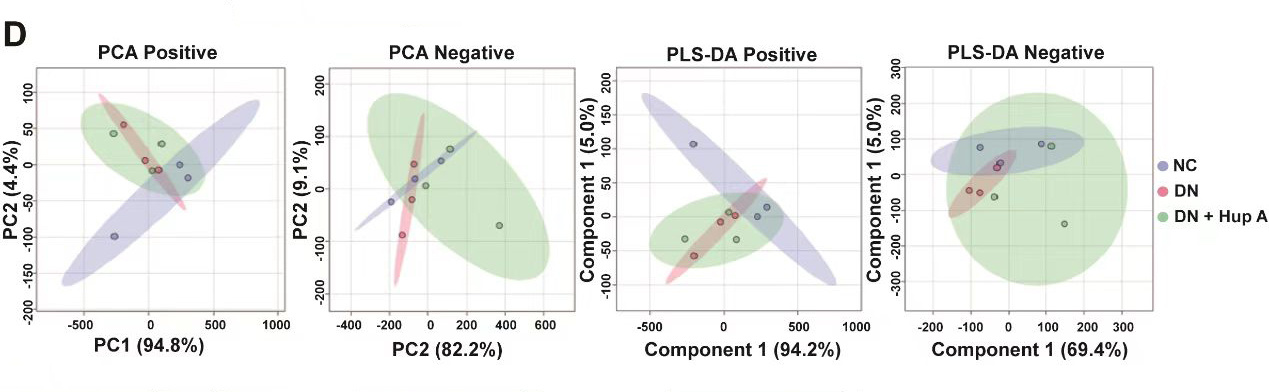
1. Renoprotective Effects: In clinical settings, urinary protein is a critical indicator for assessing kidney function and damage, often serving as a key marker for kidney disease. Studies have shown that, following administration of huperzine A to male SD rats with diabetic nephropathy (DN), rats treated with huperzine A exhibited reduced levels of urinary albumin (uALB) compared to the control group of DN rats that did not receive huperzine A. Additionally, the treatment was associated with improvements in kidney index, serum creatinine (SCr), and blood urea nitrogen (BUN) levels (as illustrated below).
(Note: NC refers to normal rats; DN refers to rats with DN; DN+Hup A refers to DN rats treated with huperzine A.)
Additionally, structural damage to the rat glomeruli and renal tubules was also alleviated under huperzine A treatment. Moreover, the protein levels of nephrin and podocin—key components essential for maintaining normal glomerular filtration function—significantly increased after administration of huperzine A.
Compared to DN rats not treated with medication, the renal function indicators and structural damage in rats treated with huperzine A were significantly improved. Therefore, it can be concluded that huperzine A exerts a protective effect on the kidneys.
2. Impact on Gene Expression: To investigate the molecular mechanisms underlying huperzine A's treatment of DN, the study conducted transcriptome sequencing and differential expression gene (DEG) analysis on kidney tissues. The results showed that ApoE and ApoC2, which were significantly upregulated in the DN group, were markedly reduced after huperzine A treatment.
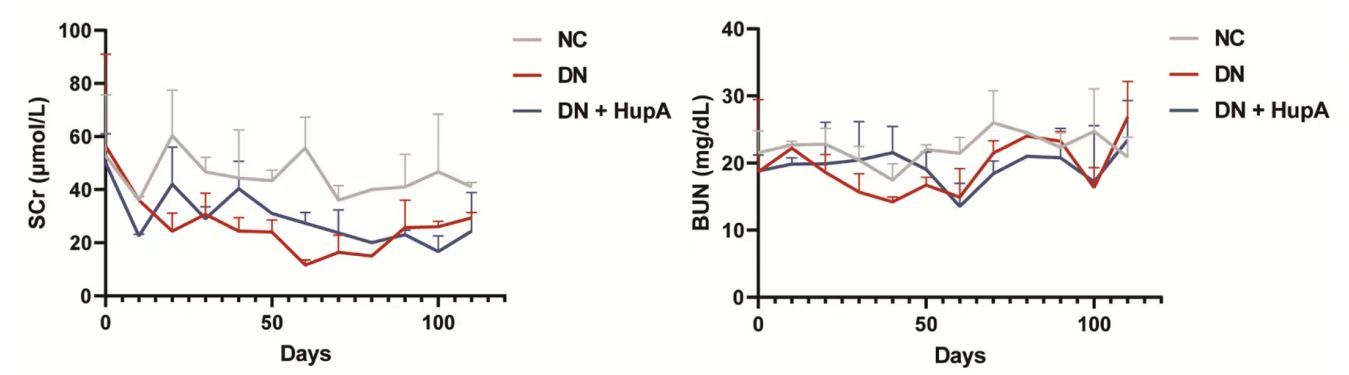
3. Metabolite Regulation: Studies using Principal Component Analysis (PCA) and Partial Least Squares Discriminant Analysis (PLS-DA) revealed significant metabolic differences between the kidney samples from the NC group and the DN group, with the DN+Hup A group showing a distribution more closely aligned with the NC group. This indicates that renal metabolism in DN rats treated with huperzine A was notably closer to that of normal rats compared to untreated DN rats. These findings suggest that huperzine A treatment partially restored metabolic functions in DN rats. (See figure below.)
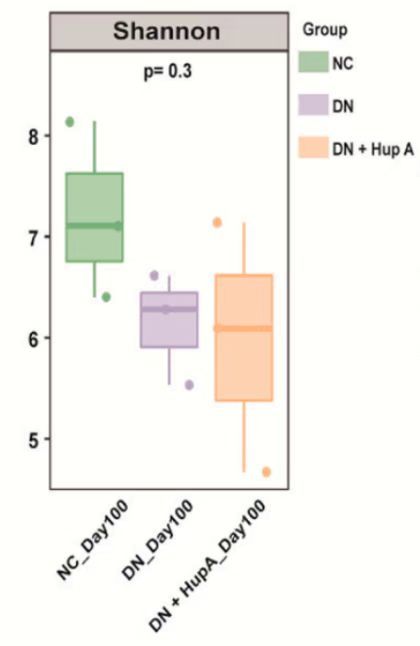
4. Improvement in Gut Microbiota: The Shannon index is a widely used metric to assess the diversity or richness of microbial communities—higher values indicate greater community diversity. Therefore, this study employed the Shannon index to evaluate the effects of huperzine A on the gut microbiota of rats. The results showed that the Shannon diversity index was reduced in the DN group but increased in the DN + Hup A group, suggesting that huperzine A treatment effectively modulated the diversity of the rat gut microbiota. (See figure below.)
Clinical significance: ApoE as a biomarker
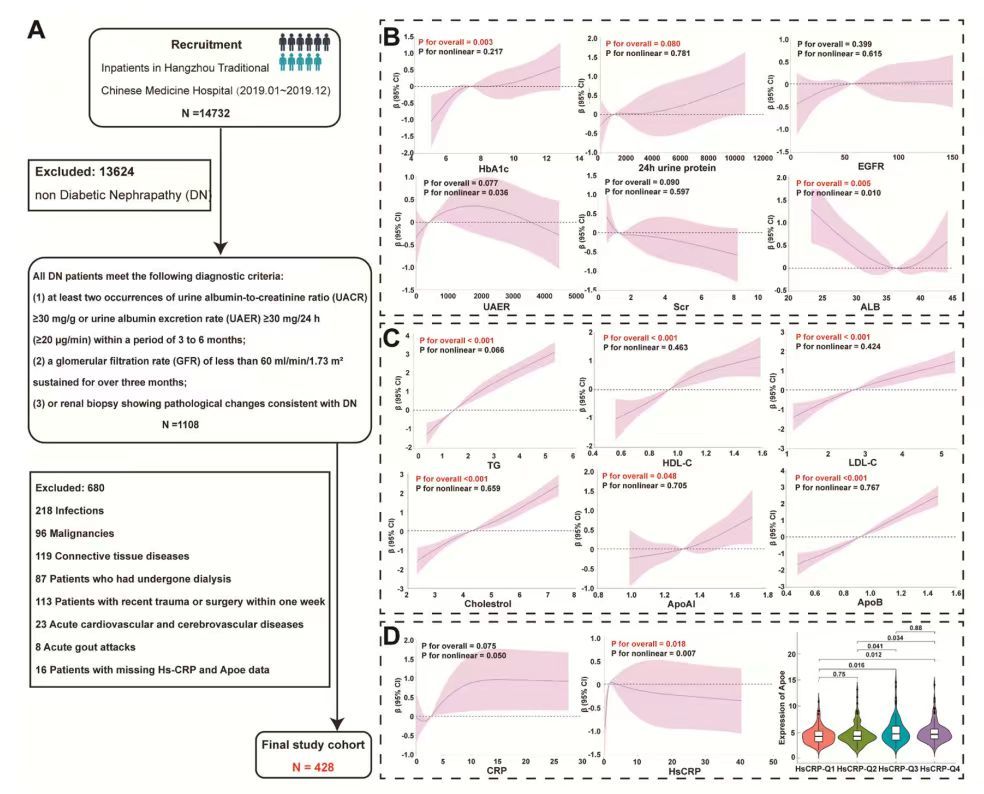
To investigate the clinical relevance of ApoE and DN-related biomarkers, the study included 428 DN patients for further analysis.
Glycated hemoglobin (HbA1c) is an important indicator of blood glucose control, and it is generally believed that HbA1c levels effectively reflect average blood sugar levels over the past 8 to 12 weeks. Research has shown that HbA1c is positively correlated with ApoE, suggesting that ApoE expression increases as HbA1c levels rise.
In terms of renal function, at high levels of proteinuria, ApoE expression showed a strong positive correlation with 24-hour urinary protein levels, indicating that ApoE expression increases as proteinuria rises.
Additionally, the study found that ApoE is significantly correlated with serum albumin (ALB), lipid biomarkers, and inflammatory markers—particularly CRP and Hs-CRP—as shown in the figure below.
The study also conducted ApoE knockdown validation, which resulted in reduced inflammation, increased cell adhesion, and enhanced cell viability. Compared to the NC group, the knockdown group showed a significant decrease in the expression of LC3B II/LC3B I protein, a marker of autophagosomes, suggesting that glucose induces higher levels of autophagy, while ApoE knockdown attenuates this process.
Network pharmacology: Validating huperzine A Multi-target action
Through network pharmacology analysis, researchers further confirmed that huperzine A may exert its effects by targeting and regulating multiple genes and metabolic pathways associated with DN, while also providing protective benefits by modulating cellular apoptosis.
Conclusion: The Potential of Huperzine A With Future Research Directions
This study provides, for the first time, evidence of huperzine A's therapeutic effects in treating DN, suggesting that huperzine A could potentially serve as a promising drug for both preventing and treating DN by targeting and regulating ApoE. Although the research has yielded encouraging results, further clinical trials and large-scale multi-omics data validation are still needed to fully assess huperzine A's clinical therapeutic potential.
Treating diabetic kidney disease is a complex process, but this research has provided us with fresh perspectives and renewed hope. As the study progresses, we look forward to huperzine A becoming a promising new solution for diabetes patients. Let’s stay tuned to the latest advancements in this field, bringing more hope and options to those living with diabetes.
Sources of research literature:
Statement:
1. This news item aims to share cutting-edge academic developments and is intended solely for healthcare professionals to review for scholarly purposes—not for advertising use.
2. Wanbangde Pharmaceutical does not recommend any medications and/or indications.
Related Recommendations
