
News
[Literature Review] Huperzine A Improves Neurological Deficits After Spontaneous Subarachnoid Hemorrhage by Inhibiting Endothelial Cell Pyroptosis
Date:
03 Jun,2024
Recently, "Huperzine A ameliorates neurological deficits after spontaneous subarachnoid hemorrhage through endothelial cell pyroptosis inhibition" was published in Acta Biochimica et Biophysica Sinica. The study was conducted by a team from the Department of Neurosurgery and the Health Checkup Center at Hangzhou First People's Hospital, affiliated with the School of Medicine at Westlake University. The study shows that huperzine A injection can inhibit endothelial cell pyroptosis, combat oxidative stress, and improve early brain injury following subarachnoid hemorrhage (SAH).
Background Introduction
Subarachnoid hemorrhage (SAH) is a severe type of stroke [1,2], primarily caused by aneurysm rupture, and is characterized by high rates of morbidity and mortality [3]. Moreover, survivors often experience cognitive impairments that significantly impact their daily functioning, work capacity, and overall quality of life [4]. Early brain injury occurring within the first 72 hours is widely recognized as the main contributor to the poor prognosis observed in SAH patients [5]. Reducing early brain damage not only improves survival rates but also enhances the long-term outcomes for SAH patients [6,7]. Therefore, preventing early brain injury in SAH patients represents a crucial therapeutic strategy aimed at improving their overall prognosis. It has been shown that neuronal apoptosis and blood-brain barrier (BBB) disruption are hallmark events associated with early brain injury following SAH. These processes are closely linked to irreversible acute brain damage after SAH and play a significant role in determining the poor prognosis experienced by many patients [8,9]. Additionally, increased BBB permeability allows immune molecules to infiltrate the brain parenchyma, further exacerbating brain injury. As such, inhibiting BBB dysfunction is considered a promising approach to effectively mitigate early brain injury after SAH, making it a key therapeutic method for enhancing patient outcomes and improving prognosis.
Subarachnoid hemorrhage (SAH) is a severe type of stroke [1, 2], primarily caused by the rupture of intracranial aneurysms, and is characterized by high rates of disability and mortality [3]. Moreover, survivors often experience cognitive impairments that significantly impact their daily functioning, work capacity, and quality of life [4]. Early brain injury occurring within 72 hours after SAH is widely recognized as one of the key factors contributing to poor patient outcomes [5]. Reducing this early brain damage not only enhances survival rates but also improves long-term prognosis for SAH patients [6, 7]. Therefore, mitigating early brain injury in SAH patients represents a crucial therapeutic strategy for optimizing their overall prognosis. Research has shown that neuronal apoptosis and blood-brain barrier (BBB) disruption are hallmark events in the early stages of SAH-induced brain injury, closely linked to irreversible acute brain damage following SAH—and serve as major determinants of unfavorable patient outcomes [8, 9]. Additionally, increased BBB permeability allows immune molecules to migrate into the brain parenchyma, further exacerbating tissue damage. Studies indicate that inhibiting BBB dysfunction can effectively alleviate early brain injury after SAH, making it a vital approach to improving patient outcomes.
Materials and Methods
Animal handling
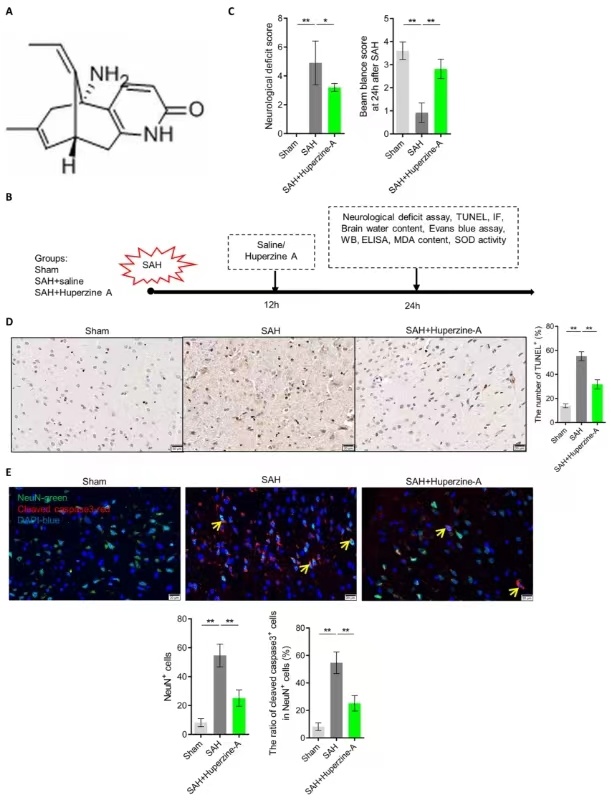
SPF male SD rats were fed according to a standard animal care protocol. After a one-week adaptation period, the following treatments were administered: (1) Sham group: SD rats underwent a sham surgery; (2) Model group: SD rats were subjected to SAH and received an intraperitoneal injection of saline; and (3) Treatment group: SD rats with SAH were treated with Huperzine A (0.1 mg/kg, WEPON, Drug Approval Number: H20183340), also administered via intraperitoneal injection. The procedure was conducted as follows: After the SD rats were anesthetized, 0.35 mL of fresh autologous blood (collected over 20 seconds) without heparin was slowly injected into the anterior cistern near the optic chiasm. The animals were then kept in a head-down position at 30°C for 20 minutes. Immediately afterward, they were injected with 2 mL of normal saline and returned to their cages individually. Body temperature was maintained at 37°C throughout the experiment. In the sham group, male SD rats weighing 250–300 g received an intraperitoneal injection of normal saline instead of autologous blood. In both the model and treatment groups, the placebo (saline) or Huperzine A was administered intraperitoneally 12 hours after the autologous blood injection.
SPF male SD rats were housed according to a standard animal care protocol. After a one-week acclimatization period, the following procedures were performed: (1) Sham-operated group: SD rats underwent a sham surgical procedure; (2) Model group: SD rats were induced with subarachnoid hemorrhage (SAH), followed by intraperitoneal injection of normal saline; (3) Treatment group: SD rats were subjected to SAH induction and then received an intraperitoneal injection of huperzine A (0.1 mg/kg, provided by Wanbangde Pharmaceutical Group Co., Ltd., Drug Approval No.: H20183340). The experimental steps are as follows: After anesthesia, fresh autologous blood without heparin was slowly injected into the pre-chiasmatic cistern over 20 seconds at a volume of 0.35 mL. The animals were kept with their heads tilted downward at 30°C for 20 minutes. Immediately afterward, 2 mL of normal saline was administered, and the rats were returned individually to their cages, with body temperature maintained at 37°C. In the sham-operated group, male SD rats weighing 250–300 g received an intraperitoneal injection of normal saline instead of autologous blood. In both the model and treatment groups, rats were given either a placebo (normal saline) or huperzine A via intraperitoneal injection, respectively, 12 hours after the autologous blood injection.
Research findings
1. Huperzine A improves neurological deficits and reduces neuronal apoptosis in brain tissue of SAH rats.
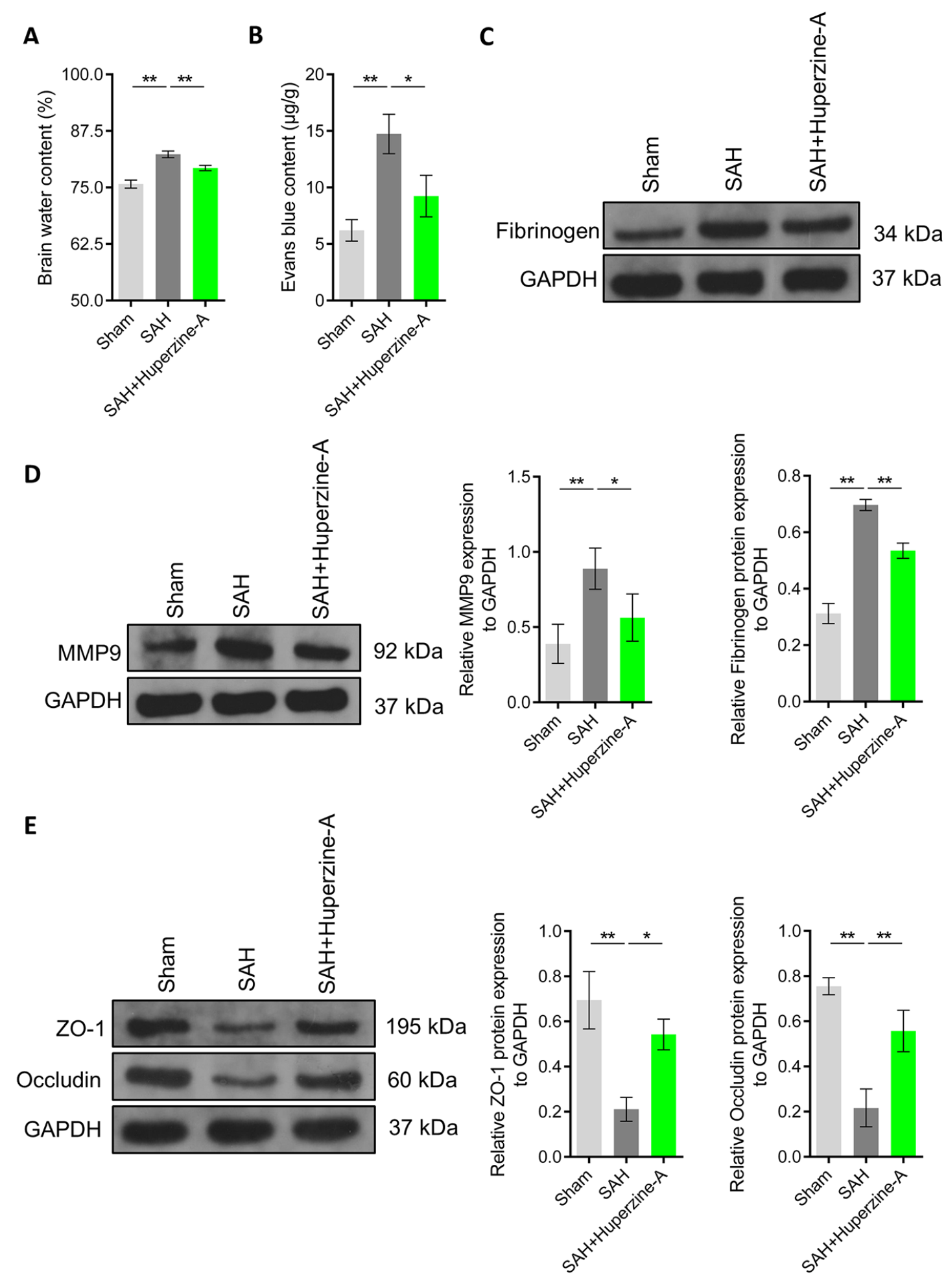
2. Huperzine A inhibits BBB dysfunction by improving the expression of tight junction proteins in SAH rats.
3. Huperzine A improved pyroptosis in endothelial cells of brain tissue in SAH rats.
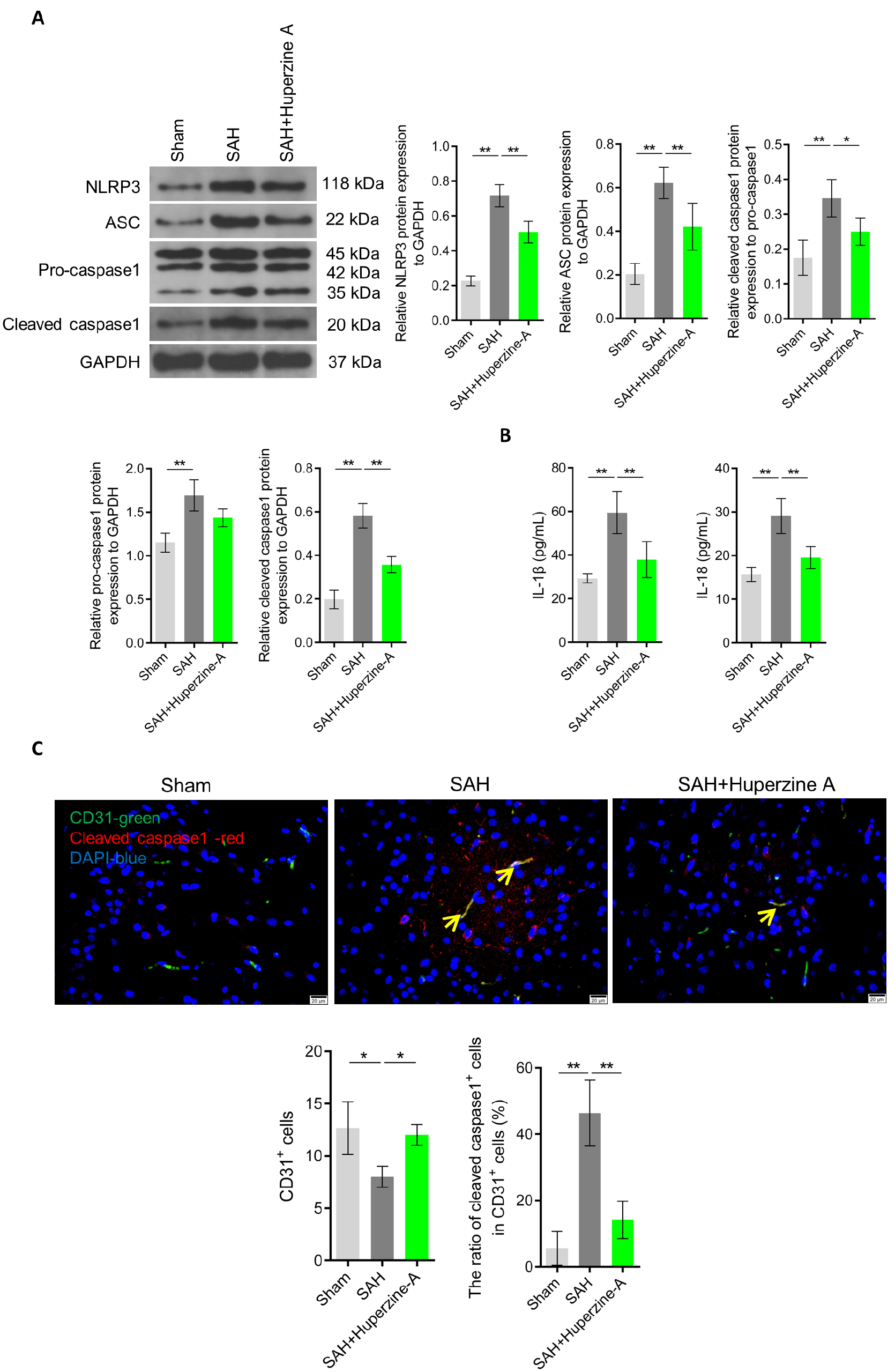
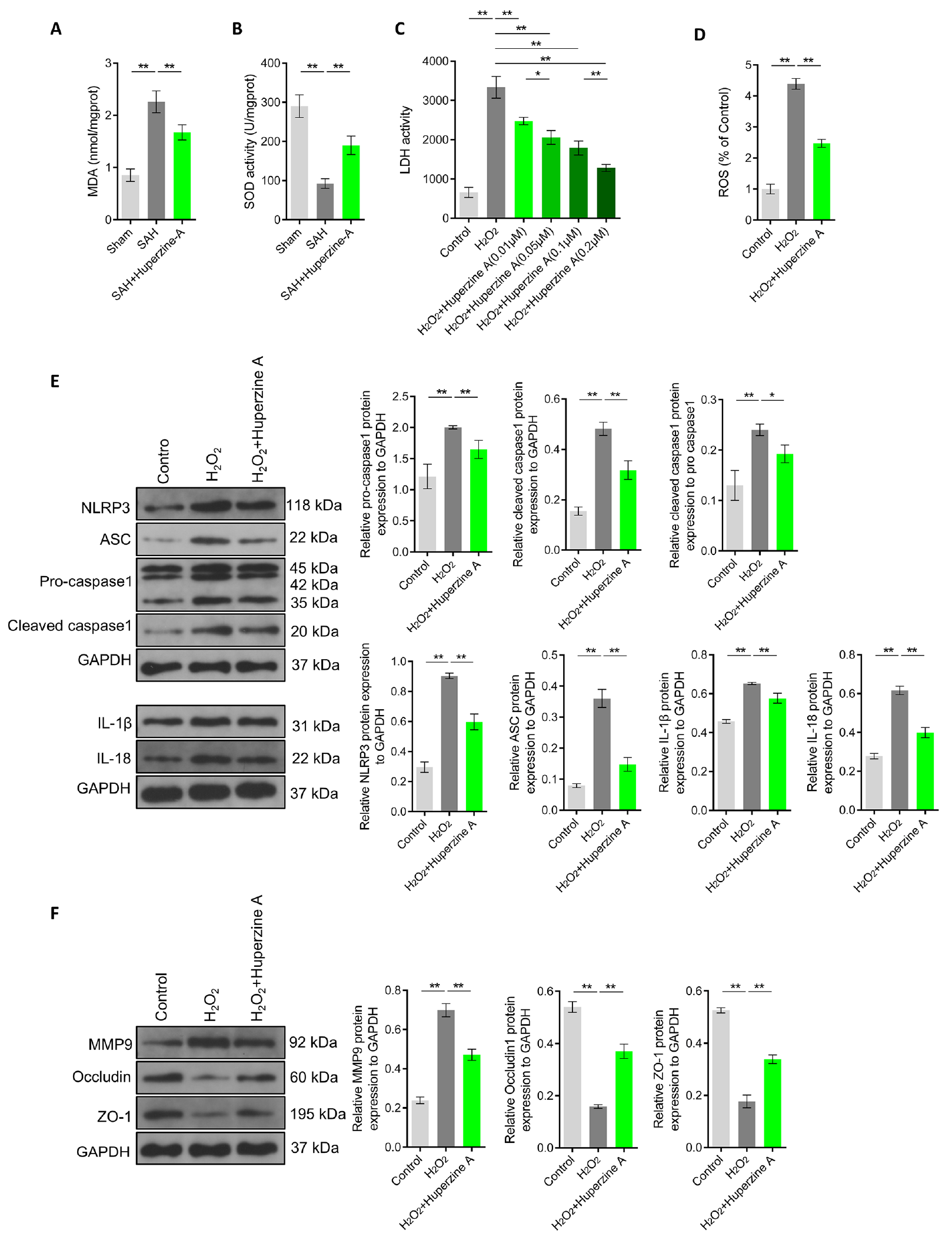
4. Huperzine A improved oxidative stress in the brain tissue of SAH rats and inhibited endothelial cell pyroptosis mediated by oxidative stress.
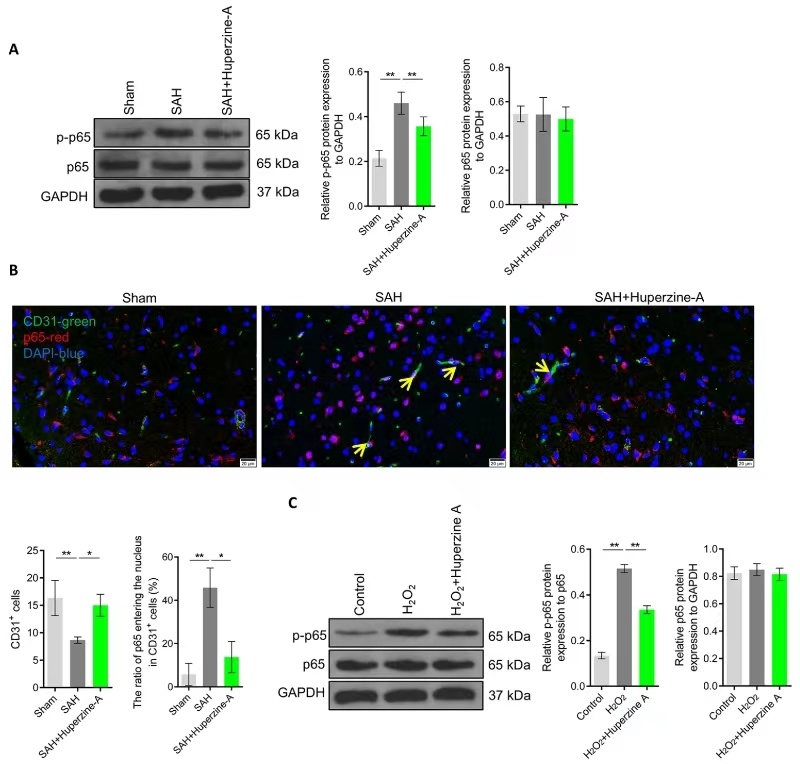
5. Huperzine A inhibits the activation of the NF-κB pathway in endothelial cells of brain tissue in SAH rats.
Conclusion: Plant-derived huperzine A exerts neuroprotective effects in obesity-related cognitive impairment [32], Alzheimer’s disease and other forms of dementia [33], as well as in repetitive traumatic brain injury [34]. In this study, we found that huperzine A significantly improved both the neurological deficit scores and balance assessments in rats subjected to SAH. Notably, huperzine A’s ability to ameliorate neuronal damage has been linked to its inhibitory effect on neuronal apoptosis [17, 18]. Consistent with these findings, our research revealed that huperzine A markedly reduced levels of neuronal apoptosis in brain tissue following SAH. These results suggest that huperzine A not only suppresses neuronal cell death but also helps mitigate early neurological deficits after SAH. Importantly, huperzine A has already been demonstrated to be safe in multiple clinical studies. This study further underscores huperzine A’s neuroprotective role in neurological disorders, offering a promising new therapeutic approach for addressing early brain injury following SAH.
References
1. Suzuki H, Hasegawa Y, Chen W, Kanamaru K, Zhang JH. Recombinant osteopontin in cerebral vasospasm after subarachnoid hemorrhage. Ann Neurol. 2010; 68: 650-60.
2. Zhang X, Karuna T, Yao ZQ, Duan CZ, Wang XM, Jiang ST, et al. High wall shear stress beyond a certain range in the parent artery could predict the risk of anterior communicating artery aneurysm rupture at follow-up. J Neurosurg. 2018; 131: 868-75.
3. Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. 2017; 389: 655-66.
4. Plata-Bello J, Modrono C, Acosta-Lopez S, Perez-Martin Y, Marcano F, Garcia-Marin V, et al. Subarachnoid hemorrhage and visuospatial and visuoperceptive impairment: disruption of the mirror neuron system. Brain Imaging Behav. 2017; 11: 1538-47.
5. Suzuki H, Nakano F. To Improve Translational Research in Subarachnoid Hemorrhage. Transl Stroke Res. 2018; 9: 1-3.
6. Fujii M, Yan J, Rolland WB, Soejima Y, Caner B, Zhang JH. Early brain injury, an evolving frontier in subarachnoid hemorrhage research. Transl Stroke Res. 2013; 4: 432-46.
7. Zhang H, He X, Wang Y, Sun X, Zhu L, Lei C, et al. Neuritin attenuates early brain injury in rats after experimental subarachnoid hemorrhage. Int J Neurosci. 2017; 127: 1087-95.
8. Lublinsky S, Major S, Kola V, Horst V, Santos E, Platz J, et al. Early blood-brain barrier dysfunction predicts neurological outcome following aneurysmal subarachnoid hemorrhage. EBioMedicine. 2019; 43: 460-72.
9. Ostrowski RP, Colohan AR, Zhang JH. Molecular mechanisms of early brain injury after subarachnoid hemorrhage. Neurol Res. 2006; 28: 399-414.
10. Chang D, Liu J, Bilinski K, Xu L, Steiner GZ, Seto SW, et al. Herbal Medicine for the Treatment of Vascular Dementia: An Overview of Scientific Evidence. Evid Based Complement Alternat Med. 2016; 2016: 7293626.
11. Ferreira A, Rodrigues M, Fortuna A, Falcão A, Alves G. Huperzine A from Huperzia serrata: a review of its sources, chemistry, pharmacology and toxicology. Phytochemistry Reviews. 2016; 15: 51-85.
12. Hao Z, Liu M, Liu Z, Lv D. Huperzine A for vascular dementia. Cochrane Database Syst Rev. 2009: CD007365.
13. Xing SH, Zhu CX, Zhang R, An L. Huperzine a in the treatment of Alzheimer's disease and vascular dementia: a meta-analysis. Evid Based Complement Alternat Med. 2014; 2014: 363985.
14. Yang G, Wang Y, Tian J, Liu JP. Huperzine A for Alzheimer's disease: a systematic review and meta-analysis of randomized clinical trials. PLoS One. 2013; 8: e74916.
15. Yue J, Dong BR, Lin X, Yang M, Wu HM, Wu T. Huperzine A for mild cognitive impairment. Cochrane Database Syst Rev. 2012; 12: CD008827.
16. Yu P, Dong WP, Tang YB, Chen HZ, Cui YY, Bian XL. Huperzine A lowers intraocular pressure via the M3 mAChR and provides retinal neuroprotection via the M1 mAChR: a promising agent for the treatment of glaucoma. Ann Transl Med. 2021; 9: 332.
17. Zhou J, Tang XC. Huperzine A attenuates apoptosis and mitochondria-dependent caspase-3 in rat cortical neurons. FEBS Lett. 2002; 526: 21-5.
18. Xiao XQ, Zhang HY, Tang XC. Huperzine A attenuates amyloid beta-peptide fragment 25-35-induced apoptosis in rat cortical neurons via inhibiting reactive oxygen species formation and caspase-3 activation. J Neurosci Res. 2002; 67: 30-6.
19. Wang Y, Wei Y, Oguntayo S, Doctor BP, Nambiar MP. A combination of [+] and [-]-Huperzine A improves protection against soman toxicity compared to [+]-Huperzine A in guinea pigs. Chem Biol Interact. 2013; 203: 120-4.
20. Ruan Q, Hu X, Ao H, Ma H, Gao Z, Liu F, et al. The neurovascular protective effects of huperzine A on D-galactose-induced inflammatory damage in the rat hippocampus. Gerontology. 2014; 60: 424-39.
21. Zhang XS, Wu Q, Wu LY, Ye ZN, Jiang TW, Li W, et al. Sirtuin 1 activation protects against early brain injury after experimental subarachnoid hemorrhage in rats. Cell Death Dis. 2016; 7: e2416.
22. Zhu Q, Enkhjargal B, Huang L, Zhang T, Sun C, Xie Z, et al. Aggf1 attenuates neuroinflammation and BBB disruption via PI3K/Akt/NF-kappaB pathway after subarachnoid hemorrhage in rats. J Neuroinflammation. 2018; 15: 178.
23. Yu LM, Zhang WH, Han XX, Li YY, Lu Y, Pan J, et al. Hypoxia-Induced ROS Contribute to Myoblast Pyroptosis during Obstructive Sleep Apnea via the NF-kappaB/HIF-1alpha Signaling Pathway. Oxid Med Cell Longev. 2019; 2019: 4596368.
24. Zhang Y, Yin K, Wang D, Wang Y, Lu H, Zhao H, et al. Polystyrene microplastics-induced cardiotoxicity in chickens via the ROS-driven NF-kappaB-NLRP3-GSDMD and AMPKPGC-1alpha axes. Sci Total Environ. 2022; 840: 156727.
25. Mo J, Enkhjargal B, Travis ZD, Zhou K, Wu P, Zhang G, et al. AVE 0991 attenuates oxidative stress and neuronal apoptosis via Mas/PKA/CREB/UCP-2 pathway after subarachnoid hemorrhage in rats. Redox Biol. 2019; 20: 75-86.
26. Zhang Y, Yang X, Ge X, Zhang F. Puerarin attenuates neurological deficits via Bcl-2/Bax/cleaved caspase-3 and Sirt3/SOD2 apoptotic pathways in subarachnoid hemorrhage mice. Biomed Pharmacother. 2019; 109: 726-33.
27. McLarnon JG. A Leaky Blood-Brain Barrier to Fibrinogen Contributes to Oxidative Damage in Alzheimer's Disease. Antioxidants (Basel). 2021; 11.
28. Qin W, Li J, Zhu R, Gao S, Fan J, Xia M, et al. Melatonin protects blood-brain barrier integrity and permeability by inhibiting matrix metalloproteinase-9 via the NOTCH3/NF-kappaB pathway. Aging (Albany NY). 2019; 11: 11391-415.
29. Wu X, Zhang H, Qi W, Zhang Y, Li J, Li Z, et al. Nicotine promotes atherosclerosis via ROS-NLRP3-mediated endothelial cell pyroptosis. Cell Death & Disease. 2018; 9: 171.
30. Wang Y, Guan X, Gao CL, Ruan W, Zhao S, Kai G, et al. Medioresinol, a novel PGC-1alpha activator, prevents pyroptosis of endothelial cells in ischemic stroke by modulating the PPARalpha-GOT1 axis. Pharmacol Res. 2021; 169: 105640.
31. Sul OJ, Ra SW. Quercetin Prevents LPS-Induced Oxidative Stress and Inflammation by Modulating NOX2/ROS/NF-κB in Lung Epithelial Cells. Molecules. 2021; 26.
32. Wang HY, Wu M, Diao JL, Li JB, Sun YX, Xiao XQ. Huperzine A Ameliorates Obesity-Related Cognitive Performance Impairments Involving the Neuronal Insulin Signaling Pathway in Mice. Acta Pharmacologica Sinica. 2020; 41: 145-53.
33. Damar U, Gersner R, Johnstone JT, Schachter S, Rotenberg A. Huperzine A as a neuroprotective and antiepileptic drug: a review of preclinical research. Expert Rev Neurother. 2016; 16: 671-80.
34. Mei Z, Zheng P, Tan X, Wang Y, Situ B. Huperzine A Alleviates Neuroinflammation, Oxidative Stress, and Improves Cognitive Function Following Repetitive Traumatic Brain Injury. Metab Brain Dis. 2017; 32: 1861-9.
35. Okada T, Kawakita F, Nishikawa H, Nakano F, Liu L, Suzuki H. Selective Toll-Like Receptor 4 Antagonists Prevent Acute Blood-Brain Barrier Disruption After Subarachnoid Hemorrhage in Mice. Mol Neurobiol. 2019; 56: 976-85.
36. Okada T, Enkhjargal B, Travis ZD, Ocak U, Tang J, Suzuki H, et al. FGF-2 Attenuates Neuronal Apoptosis via the FGFR3/PI3K/Akt Signaling Pathway Following Subarachnoid Hemorrhage. Mol Neurobiol. 2019; 56: 8203–19.
37. Sabri M, Lass E, Macdonald RL. Early brain injury: a common mechanism in subarachnoid hemorrhage and global cerebral ischemia. Stroke Res Treat. 2013; 2013:394036.
38. Suzuki H. What is early brain injury? Transl Stroke Res. 2015; 6: 1-3. 39. Sabri M, Ai J, Lass E, D'Abbondanza J, Macdonald RL. Genetic elimination of eNOS reduces secondary complications of experimental subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2013; 33: 1008-14.
40. Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol. 2015; 7: a020412.
41. Huang L, Chen Y, Liu R, Li B, Fei X, Li X, et al. P-Glycoprotein Exacerbates Blood-Brain Barrier Dysfunction in Experimental Ischemic Stroke by Inhibiting Endothelial Autophagy. Aging Dis. 2022; 13: 1546-61.
42. Heithoff BP, George KK, Phares AN, Zuidhoek IA, Munoz-Ballester C, Robel S. Astrocytes are essential for maintaining the blood-brain barrier in the adult mouse brain. Glia. 2021; 69: 436-72.
43. Zhang S, An Q, Wang T, Gao S, Zhou G. Autophagy- and MMP-2/9-Mediated Reduction and Redistribution of ZO-1 Contribute to Hyperglycemia-Induced Increased Blood-Brain Barrier Permeability During Early Reperfusion in Stroke. Neuroscience. 2018; 377: 126-37.
44. Xu P, Tao C, Zhu Y, Wang G, Kong L, Li W, et al. TAK1 Mediates Neuronal Pyroptosis in Early Brain Injury Following Subarachnoid Hemorrhage. J Neuroinflammation. 2021; 18: 188.
45. Xu P, Hong Y, Xie Y, Yuan K, Li J, Sun R, et al. TREM-1 Exacerbates Neuroinflammatory Injury via NLRP3 Inflammasome-Mediated Pyroptosis in Experimental Subarachnoid Hemorrhage. Transl Stroke Res. 2021; 12: 643-59.
46. Liu L, Wang N, Kalionis B, Xia S, He Q. HMGB1 plays a critical role in pyroptosis-induced blood-brain barrier disruption in diabetes-associated cognitive decline. J Neuroimmunol. 2022; 362: 577763.
47. Bellut M, Papp L, Bieber M, Kraft P, Stoll G, Schuhmann MK. NLPR3 inflammasome inhibition alleviates hypoxic endothelial cell death in vitro and protects blood-brain barrier integrity in murine stroke. Cell Death Dis. 2021; 13: 20.
48. Liang Y, Song P, Chen W, Xie X, Luo R, Su J, et al. Inhibition of Caspase-1 Alleviates Ischemia-Associated Blood-Brain Barrier Dysfunction and Impairment by Suppressing Pyroptosis Activation. Front Cell Neurosci. 2020; 14: 540669.
49. Matz PG, Copin JC, Chan PH. Cell death following exposure to subarachnoid hemolysate correlates inversely with the expression of CuZn-superoxide dismutase. Stroke. 2000; 31:2450-9.
50. Marzatico F, Gaetani P, Cafe C, Spanu G, Rodriguez y Baena R. Antioxidant Enzymatic Activities Following Experimental Subarachnoid Hemorrhage in Rats. Acta Neurol Scand. 1993; 87: 62-6.
51. Zheng D, Liu J, Piao H, Zhu Z, Wei R, Liu K. ROS-Triggered Mechanisms of Endothelial Cell Death: Focus on Pyroptosis, Parthanatos, and Ferroptosis. Front Immunol. 2022; 13: 1039241.
52. Xiao XQ, Wang R, Han YF, Tang XC. Protective effects of huperzine A on beta-amyloid (25-35)-induced oxidative damage in rat pheochromocytoma cells. Neurosci Lett. 2000; 286: 155-8.
53. Tao LX, Huang XT, Chen YT, Tang XC, Zhang HY. Huperzine A's acetylcholinesterase-independent protective effects against oxidative damage and aberrant iron metabolism signaling induced by iron overload in rat cortical neurons. Acta Pharmacol Sinica. 2016; 37: 1391-400.
54. Xu Z, Wang Y. Huperzine A attenuates hepatic ischemia-reperfusion injury via antioxidative and anti-apoptotic pathways. Mol Med Rep. 2014; 10: 701-6.
55. Chen J, Xuan Y, Chen Y, Wu T, Chen L, Guan H, et al. Netrin-1 attenuates subarachnoid hemorrhage-induced brain injury via the PPARgamma/NF-KB signaling pathway. J Cell Mol Med. 2019; 23: 2256-62.
56. Kolgazi M, Uslu U, Yuksel M, Velioglu-Ogunc A, Ercan F, Alican I. The role of the cholinergic anti-inflammatory pathway in acetic acid-induced colonic inflammation in rats. Chem Biol Interact. 2013; 205: 72-80.
57. Sui X, Gao C. Huperzine A alleviates damage induced by acute myocardial infarction in rats via antioxidant, anti-apoptotic, and anti-inflammatory mechanisms. Int J Mol Med. 2014; 33: 227-33.
Statement:
1. This news item aims to share cutting-edge academic developments and is intended solely for healthcare professionals to consult for academic purposes—not for advertising purposes.
2. Wanbangde Pharmaceutical does not recommend any medications and/or indications.
Related Recommendations
